Best Knee Wrap for Baker’s Cyst: A Baker’s cyst, also known as a popliteal cyst, is a fluid-filled sac that forms behind the knee. It is most commonly seen in people who have arthritis or other conditions that affect the knees. In this article, we will discuss the causes, symptoms, and treatment of baker’s cysts. We will also provide tips for preventing them from forming in the first place!
These cysts are named for the doctor who first described them. In 1854, Dr. William Morrant Baker noted that these popliteal boils resulted from fluid flowing out of a damaged knee joint and into an adjacent space around it (the subcutaneous tissue). When structures within or near your Kneecap become injured -as can happen during sports-related injuries-they produce extra fluid which then collects in this cavity leading to the formation of painful swelling known colloquially as a “Baker’s cyst”.
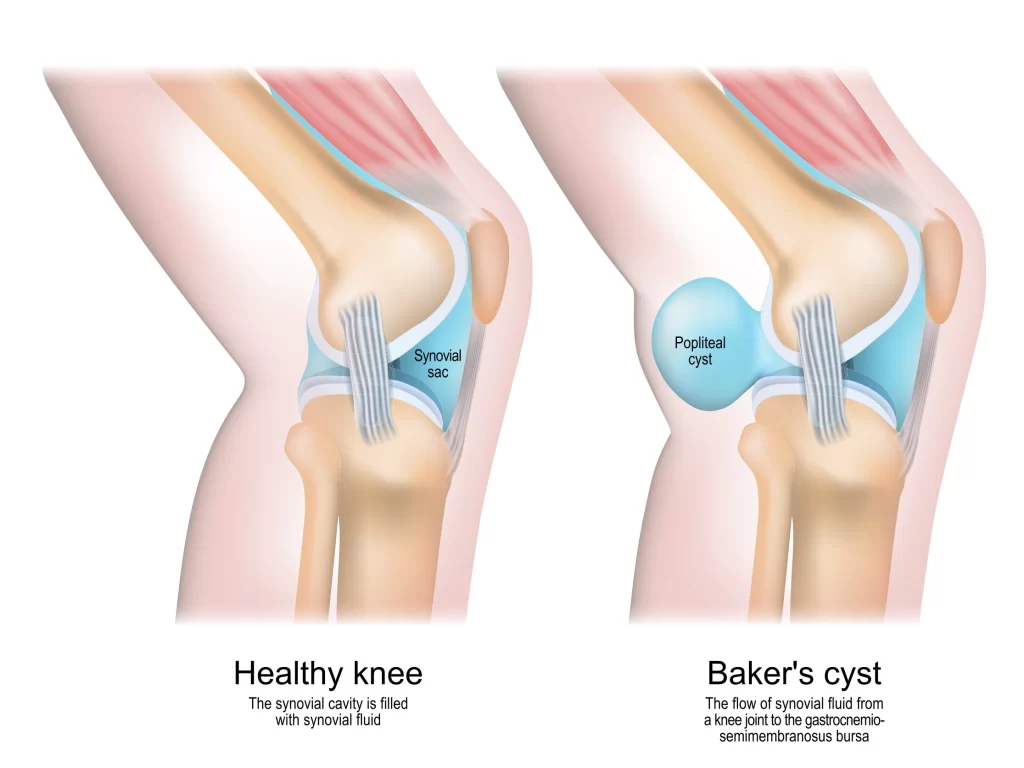
Normal Knee Anatomy
The knee is the body’s largest and most powerful joint. It includes the lower end of the femur (thighbone), upper end of the tibia (shinbone), and patella (kneecap). Articular cartilage, a smooth, slippery tissue that covers and protects the ends of the bones where they come together to form a joint, lines the ends of the bones where they meet. The knee joint is filled with a clear liquid (synovial fluid) that serves as a lubricant to help reduce friction within it. Bursas are small fluid-filled sacks that cushion the joint and aid in reducing friction between muscles and other surrounding structures.
What is a Baker’s Cyst, and What Causes it to Form
A baker’s cyst, also known as a popliteal cyst, is a type of fluid-filled sac that forms near the back of the knee. The sac is actually a section of the knee joint capsule that has become distended with fluid. Baker’s cysts occur when this fluid leaks out of the joint and into the surrounding tissue. The most common cause of a baker’s cyst is arthritis, specifically osteoarthritis or rheumatoid arthritis.
However, other conditions that can lead to the formation of a baker’s cyst include gout, meniscus tears, and ligament injuries. Baker’s cysts are relatively benign and usually do not cause any symptoms. However, they can become painful if they rupture or if they put pressure on the nerve that leads to the calf and foot.
Treatment for a baker’s cyst typically involves treating the underlying cause of the fluid buildup. In some cases, your knee doctor may consider draining the fluid from the sac. In many cases, corticosteroid injections may also be used to help reduce inflammation. In rare cases, surgery may be necessary to remove the cyst.
What are the Symptoms of a Baker’s Cyst and Synovial Fluid in the Knee
A baker cyst is a fluid-filled sacs that form near the knee joint as a result of arthritis or other ailments that harm the knee joint. The cyst may occasionally burst, resulting in synovial fluid seeping into the calf muscle, producing severe discomfort, edema, and inflammation.
You may feel no pain or only a little discomfort with a Baker’s cyst. You could just have knee discomfort from the initial damage that caused the Baker’s cyst, but not the lump itself. This swelling in your knee can make it painful to bend it.
Symptoms of a Baker’s cyst may include:
- Pain
- A fluid-filled bump behind your knee
- Knee joint stiffness
- Limited range of motion (difficulty bending the knee)
- Swelling of your knee or calf
A Baker’s cyst may produce swelling, redness, and a feeling of warmth in your lower leg that is comparable to those produced by a blood clot. A blood clot (also known as deep vein thrombosis) is an emergency situation that requires immediate medical attention. If you’re not sure whether or not you have a Baker’s cyst or a blood clot, talk to your doctor right away. Your doctor can examine your symptoms and determine if you have a Baker’s cyst or a blood clot.
How are Baker’s Cysts Diagnosed
Baker’s cysts are typically diagnosed during a physical exam. Your doctor will ask about your symptoms and feel for any bulging or tenderness behind your knee. If a Baker’s cyst is suspected, you may also have an MRI or ultrasound to confirm the diagnosis. In some cases, a Baker’s cyst may be associated with a meniscus tear. If this is suspected, your doctor may order additional tests to evaluate the meniscus.
Treatment for a Baker’s cyst typically includes rest, ice, and elevation. In some cases, you may also need to take anti-inflammatory medications or use crutches. If the Baker’s cyst does not respond to conservative treatment, you may need to have it drained surgically.
How are Baker’s Cysts Treated
Nonsurgical Treatment:
Treatment for a baker’s cyst typically involves rest, ice, and anti-inflammatory medication. Ibuprofen, paracetamol and even over-the-counter medications can help reduce the swelling in your knee. Try using an ice pack or compressive knee sleeve or brace to provide relief and help limit swelling. In general, the RICE (rest, ice, compression, elevation) principles are employed. Often physical therapy may help.

Ruptured Cyst:
A Baker’s cyst can sometimes rupture (burst), resulting in fluid leaking down into your calf. This causes a sharp pain in your calf, which becomes swollen, tight and red, but redness can be harder to see on brown and black skin. The fluid will gradually be reabsorbed into the body within a few weeks. The recommended treatment for a ruptured cyst is rest and elevation (keeping the affected leg raised).
Aspiration of Popliteal Cyst
In some cases, the cyst may need to be aspirated (drained) with a needle. This is most often done with the use of an ultrasound that lets your knee doctor visualize the cyst and cyst contents, as well as surrounding structures in the calf region. Several important structures in that area must be avoided (e.g. popliteal artery, tibial nerve). After aspiration of the fluid-filled sac, a steroid injection may be administered to help prevent it from coming back. A compression wrap is often applied to prevent the reaccumulation of too much synovial fluid.
Surgical Treatment for Popliteal Cysts
Surgery is rarely necessary. Surgically removing a Baker’s cyst is not easy because they do not have an inner lining like other types of cavities. If you sustain significant damage to your knee joint following injury or due to conditions such as osteoarthritis, surgery may be needed for treatment—and it could involve keyhole diagnosis with instruments called arthroscopes that allow the orthopedic surgeon to see deep inside the knee joint. Some examples of other treatments and surgical considerations:
- Knee arthroscopy – minimally invasive surgery using arthroscopes may allow your knee surgeon to visualize additional damage and arthritis in your knee
- Meniscus surgery – meniscus repair or partial meniscectomy may help to address any meniscal tear that could be allowing excess fluid from the joint space to seep into the back of the knee
- Cartilage restoration – cartilage repair surgeries such as MACI or BioUni may be used to address the underlying cartilage damage that is causing the knee to produce excess fluid
Prevention Tips
There are several things you can do to prevent baker’s cysts from forming in the first place. For example, if you have arthritis, it’s important to keep your joints healthy and strong with regular exercise and low-impact weight-bearing activity. Some foods help treat arthritis, and maintaining a healthy body weight is crucial.
You should also avoid activities that put too much stress on your knees, such as deep squats with heavy weight or high-impact activities. If you have a previous injury or condition that has affected your knees, it’s important to get treatment as soon as possible to prevent further damage. Finally, if you experience any swelling or stiffness in your knees, be sure to see a doctor so they can rule out any underlying medical conditions. By following these tips, you can help prevent baker’s cysts from forming in the first place.